Keeping your bones strong as you age & the role of calcium

Our bones feel so strong. They support us, protect our organs, and make us mobile. But our skeletons aren’t unchanging and permanent like the ones hanging in a science museum.
When I studied physiology I was awed by the fact that our bones are constantly remodeling and regenerating. But because we don’t really notice this process, it’s easy to forget the importance of nourishing our bones.
Calcium is the key mineral in bone remodeling and regenerating.
4 Key takeaways
- As we age, we lose calcium from our bones.
- Women tend to have smaller thinner bones than men.
- The decrease in oestrogen around menopause triggers a decline in bone density.
- The spaces in the honeycomb structure of our bones become larger and our bones become more brittle.
In its severe form this lower bone density is osteoporosis – a major risk factor for fractures which is estimated to affect 23% of women and 6% of men over 50 in Australia.*
Exercise can help
Exercise and being active is important to help reduce risks. Exercises that improve balance – like yoga or dancing reduce the risk of falling in the first place. Weight-bearing exercises such as running, hiking, or tennis help increase bone regeneration.
But our bones need calcium for that rebuilding.
How much Calcium do I need each day?
Nutritionists recommend that women older than 50 should aim for 1300 mg of calcium per day. Men should aim for 1000 mg per day until they reach 70 when the 1300 mg of calcium goal applies to them too.
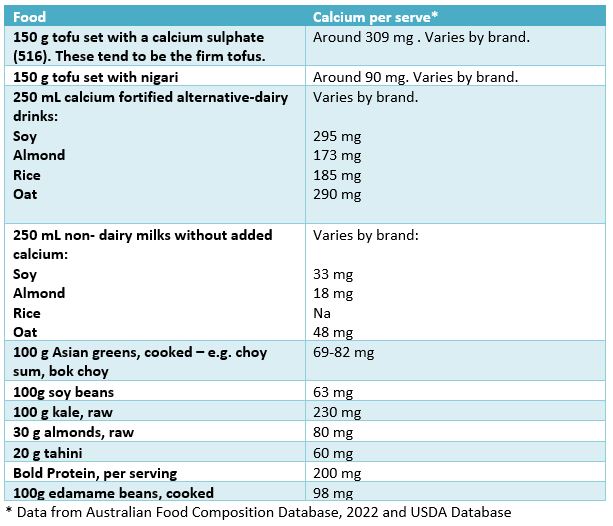
My table lists some non-dairy sources of calcium to help build stronger bones.
Dairy and calcium
Dairy foods have been a traditional source of calcium in many countries. For many reasons, dairy isn’t always the answer. Some people are vegan, some have allergies or intolerances and others are concerned about carbon emissions from dairy cows. You may just be one of those Australians scarred for life by having to drink warm milk every morning at primary school. However, recent studies have shown that non-meat eaters, especially vegans, have higher rates of fractures, including hip fractures.** While the evidence is still emerging, it seems that lower levels of dietary calcium and protein are likely causes for these fractures.
Don’t count spinach and silver beet for calcium. The oxalates in these vegetables severely limit calcium absorption to around 5%. There tend to be wide differences between fortified and non-fortified alternate dairy drinks. It pays to check the label.
A rich and varied diet is the best way to meet your calcium needs.
Products like Bold protein with added calcium make that challenge easier.
If you are concerned about your bone density, consult your GP to see all the steps you can take for stronger, healthier bones.
Louise

Sources
*Australian Institute of Health and Welfare 2014, Estimating the prevalence of osteoporosis in Australia, AIHW, Canberra.
**Tong, T.Y.N., Appleby, P.N., Armstrong, M.E.G. et al. Vegetarian and vegan diets and risks of total and site-specific fractures: results from the prospective EPIC-Oxford study. BMC Med 18, 353 (2020). https://doi.org/10.1186/s12916-020-01815-3


